Abstract
We present the case of a 41-year-old male diagnosed with high-risk prostate adenocarcinoma (initial Gleason score 4+4=8, upgraded postoperatively to 4+5=9) with sarcomatoid features. Although rare, prostate cancer in younger patients can be biologically aggressive. This report underscores the need for early detection, the utility of biparametric MRI in risk stratification, and the role of multimodal therapy—surgery, radiotherapy, and chemotherapy—in improving outcomes in young patients with high-risk disease.
Introduction
Prostate cancer is typically a disease of older men, with a median age at diagnosis of 66 years. Fewer than 2% of all prostate cancer cases occur in men younger than 50 years, but these early-onset cases may exhibit more aggressive histopathological features and worse prognosis than those in older patients.1,2 Young patients often present without significant family history or established risk factors, complicating timely diagnosis.3 Here, we present a case of early-onset prostate cancer with a high Gleason score and sarcomatoid differentiation—a rare and aggressive variant.
Case Presentation
Patient Background:
A 41-year, 3-month-old male presented with occasional hematuria and hemospermia over the past three months, along with dysuria. No fever, loin pain, or urinary urgency was reported. He had no significant family history of prostate cancer or other malignancy.
PSA Level:
Serum prostate-specific antigen was elevated at 12.0 ng/mL (measured on January 31, 2024), significantly above the expected threshold for his age.4
Clinical Findings:
- Digital Rectal Examination: A suspicious firm nodule was palpated on the right side of the prostate.
- No palpable lymphadenopathy or systemic signs of malignancy.
Imaging Studies
A biparametric MRI (bpMRI) of the prostate demonstrated:
- A 1.11 cm × 0.99 cm lesion in the right posteromedial peripheral zone at the apex.
- T2-weighted: Charcoal/erase-type hypointensity.
- DWI: Hyperintense.
- ADC map: Low signal (restricted diffusion).
The lesion was classified as PI-RADS 4, suggestive of clinically significant cancer.5 There was no evidence of extracapsular extension or seminal vesicle invasion.

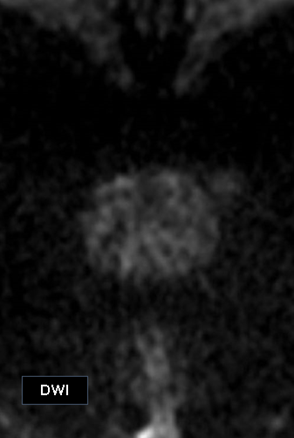
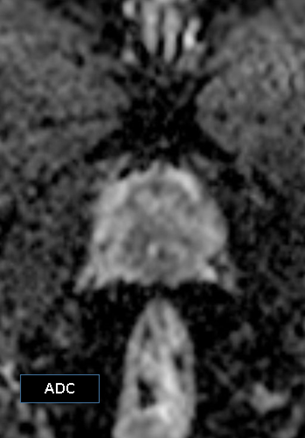
MRI findings were suggestive of clinically significant prostate cancer [Turkbey et al., 2019].
Biopsy and Histopathology
A 12-core transrectal ultrasound-guided prostate biopsy yielded the following results:
- Diagnosis: Acinar adenocarcinoma, Gleason 4+4 (Grade Group 4).
- Tumor involvement: 6 of 12 cores, bilaterally.
- Perineural invasion: Absent.
Whole-body MRI (February 20, 2024) showed no evidence of metastatic disease.
Clinical staging: cT2cN0M0.
Management
Surgical Treatment:
The patient underwent laparoscopic radical prostatectomy on March 5, 2024, under general anesthesia.
Final Pathology:
- Acinar adenocarcinoma with focal sarcomatoid differentiation.
- Upgraded Gleason score: 4+5=9 (Grade Group 5).
- Margins: Positive.
Sarcomatoid components are rare (<1% of cases) and portend a highly aggressive clinical course (6).
Adjuvant Therapy:
- Radiotherapy: 66 Gy in 33 fractions using intensity-modulated radiotherapy (IMRT) to the pelvis and postoperative bed, completed six weeks post-surgery.
- Chemotherapy: Six cycles of docetaxel and prednisolone initiated post-radiotherapy. Treatment was well tolerated without significant adverse events.
Post-Treatment Surveillance
The patient is under regular follow-up.
- He reports no urinary incontinence or obstructive symptoms.
- Most recent PSA (June 2025): 0.23 ng/mL.
- Imaging and clinical exams show no signs of recurrence.
Discussion
Prostate cancer in men younger than 50 is rare but often biologically aggressive and less likely to be suspected (1,2). A PSA value >10 ng/mL significantly increases the likelihood of high-grade disease (4). The use of bpMRI with PI-RADS scoring enhances diagnostic accuracy, especially when combined with targeted biopsy (5).
Sarcomatoid prostate carcinoma is an exceptionally aggressive histological variant associated with rapid progression and poor prognosis (6,7). Positive margins, high Gleason score, and sarcomatoid differentiation necessitate a multimodal treatment strategy, including radiotherapy and chemotherapy, to reduce recurrence risk and improve survival outcomes (8,9).
Although this patient had no known family history, early-onset and high-grade prostate cancer should prompt consideration of germline testing for BRCA1/2, HOXB13, and other mutations linked to hereditary prostate cancer syndromes (10).
Conclusion
This case highlights the importance of considering prostate cancer in younger patients presenting with urologic symptoms and elevated PSA. Early MRI-based detection, timely biopsy, aggressive surgical intervention, and adjuvant therapy contributed to disease control. Clinicians should maintain a high index of suspicion and consider genetic testing for optimal management in such cases.
Authors of this article
- Prof. Brig. Gen (Retd) Jahangir Alam, MBBS, MCPS, FCPS (Radiology), Fellow MRI (USA), Head-Radiology & Imaging Operation, Square Hospitals LTD.
- Dr. N.I. Bhuiyan, MBBS, MS (Urology), Consultant, Urology, Square Hospitals Ltd.
- Dr. Arunangshu Das, MBBS. FCPS, Consultant, Oncology, Square Hospitals Ltd.
- Dr. Shoheli Sultana, MBBS, MD, Consultant, Radiology and Imaging, Square Hospitals Ltd.
References
- Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2024. CA Cancer J Clin. 2024;74(1):7-33. doi:10.3322/caac.21805
- Pernar CH, Ebot EM, Wilson KM, Mucci LA. The epidemiology of prostate cancer. Cold Spring Harb Perspect Med. 2018;8(12):a030361. doi:10.1101/cshperspect.a030361
- Salinas CA, Tsai CJ, De Marzo AM, et al. Clinical features of young men diagnosed with prostate cancer after prostate-specific antigen testing. J Urol. 2006;175(4):1427-1431. doi:10.1016/S0022-5347(05)00697-6
- Loeb S, Carter HB, Berndt SI, Ricker W, Schaeffer EM. Complications after prostate biopsy: data from SEER-Medicare. J Urol. 2011;186(5):1830-1834. doi:10.1016/j.juro.2011.06.057
- Turkbey B, Rosenkrantz AB, Haider MA, et al. Prostate imaging reporting and data system version 2.1: 2019 update of PI-RADS. Eur Urol. 2019;76(3):340-351. doi:10.1016/j.eururo.2019.02.033
- Wang J, Wang FW, Lagrange CA, Hemstreet GP III, Kessinger A. Clinical features of sarcomatoid carcinoma (carcinosarcoma) of the prostate: a case report and review of the literature. Can J Urol. 2008;15(3):4101-4103.
- Moslemi MK, Dadkhah F. Sarcomatoid carcinoma of the prostate: A rare case and review of the literature. Urol Ann. 2013;5(1):43-46. doi:10.4103/0974-7796.106942
- Petrylak DP, Tangen CM, Hussain MHA, et al. Docetaxel and estramustine compared with mitoxantrone and prednisone for advanced refractory prostate cancer. N Engl J Med. 2004;351(15):1513-1520. doi:10.1056/NEJMoa041318
- Hoffman KE, Niu J, Shen Y, et al. Physician variation in the use of adjuvant therapies for prostate cancer. JAMA Oncol. 2019;5(6):847–855. doi:10.1001/jamaoncol.2019.0175
- Pritchard CC, Mateo J, Walsh MF, et al. Inherited DNA-repair gene mutations in men with metastatic prostate cancer. N Engl J Med. 2016;375(5):443-453. doi:10.1056/NEJMoa1603144

