Abstract
Background: Sepsis is a life-threatening condition marked by a dysregulated host immune response leading to multi-organ dysfunction. Despite advancements in critical care, sepsis-associated organ failure, particularly involving the liver and kidneys, remains a major therapeutic challenge.
Case Presentation: We report the successful use of CytoSorb hemoadsorption therapy in a 35-year-old female presenting with sepsis, acute fulminant hepatitis, and multi-organ failure. The patient was admitted with high-grade fever, jaundice, and oliguria, later developing respiratory distress and progressive hepatic and renal impairment. Initial management with broad-spectrum antibiotics and hemodialysis failed to halt clinical deterioration.
Intervention: In response to escalating organ dysfunction, CytoSorb hemoadsorption was integrated with renal replacement therapy (RRT). The patient underwent two 12-hour hemoadsorption sessions over a 48-hour period.
Outcomes: Significant clinical and biochemical improvements were observed. Serum bilirubin decreased from 24.1 mg/dL to 5.6 mg/dL, alanine aminotransferase (ALT) from 335 U/L to 59 U/L, and procalcitonin levels from 23.2 μg/L to 9.54 μg/L. Respiratory symptoms resolved, and the patient achieved hemodynamic stability. She was successfully transferred from the intensive care unit to the general ward and later discharged without complications.
Conclusion: This case illustrates the potential role of CytoSorb hemoadsorption as an adjunctive therapy in the management of complex sepsis with hepatic and renal involvement. By effectively reducing systemic inflammation and improving organ function, hemoadsorption may offer a promising therapeutic option in critically ill patients. Further large-scale studies are needed to validate its clinical efficacy, long-term outcomes, and cost-effectiveness.
Key Words: CytoSorb, Cytokines, Hemoadsorption, Sepsis, Septic shock
Introduction
Sepsis, a life-threatening organ dysfunction caused by a dysregulated host response to infection, is often complicated by multi-organ failure, including acute kidney injury (AKI) and liver dysfunction.1,2 Managing sepsis remains challenging due to the complex interplay of inflammation, immune dysregulation, and organ impairment. Cytokine adsorption therapy, such as hemoadsorption using CytoSorb, has emerged as a promising adjunct to conventional treatments in sepsis.3 Hemoadsorption works by removing excess cytokines, bilirubin, and other inflammatory mediators from circulation using porous polymer beads. This mechanism helps modulate the immune response, reduce inflammation, and support organ recovery.
In particular, CytoSorb has shown utility in patients with AKI and liver dysfunction, where its adsorptive capacity aids in decreasing inflammatory markers and improving excretory liver function.4,5 This case report illustrates the effectiveness of hemoadsorption therapy in the rapid stabilization and organ recovery of a patient with sepsis, acute fulminant hepatitis, and multi-organ failure.
Case Presentation
On January 4, 2024, a 35-year-old female arrived at a peripheral hospital with a 7-day history of fever, yellowish discoloration of the skin, sclera, and urine, and severe pruritus. She disclosed that she had taken herbal medications along with nonsteroidal anti-inflammatory drugs. Her symptoms complicated further as she developed oliguria as time progressed. Hyperbilirubinemia (15.2 mg/dl), leukocytosis (44.80 K/μl), elevated erythrocyte sedimentation rate (41 mm/hour), and altered liver enzymes (SGPT/ALT 450 U/L, ALP 902 U/L) were all identified during the initial laboratory investigations. Intravenous ceftriaxone was administered as initial therapy.
Her condition worsened with a rise in serum creatinine to 7.1 mg/dl, necessitating haemodialysis on January 6. Subsequently, she developed respiratory distress and somnolence and was referred to BIRDEM General Hospital, Dhaka, on January 8. Upon admission, she was conscious but somnolent and required oxygen supplementation via nasal cannula. Bilateral pulmonary crepitations were noted on auscultation. Laboratory findings included serum bilirubin 24.1 mg/dl, procalcitonin (PCT) 23.2 μg/l, serum creatinine 9.7 mg/dl, ferritin 2268 ng/ml, and serum potassium 6.3 mEq/L. A chest X-ray revealed bilateral pulmonary oedema. Hepatitis serologies were negative, but ANA was positive, suggesting an autoimmune component. Given her complex presentation involving sepsis, AKI, and acute fulminant hepatitis, the medical team initiated hemoadsorption therapy using CytoSorb in conjunction with renal replacement therapy (RRT).
Treatment
Two 12-hour sessions of hemoadsorption therapy were performed over 48 hours with a 24-hour interval between sessions. CytoSorb was integrated with RRT (White, 2007) without anticoagulation, given the elevated risk of bleeding in the setting of liver dysfunction. The hemoadsorber was positioned pre-hemofilter, with blood flow and dialysate flow rates set at 150 ml/min and 2000 ml/min, respectively. Concurrent antibiotic therapy with meropenem and moxifloxacin was administered.
Measurements
Clinical and laboratory parameters, including bilirubin, liver enzymes (ALT/SGPT, AST/SGOT), PCT, and consciousness levels, were closely monitored. A timeline of key lab parameter trends is provided in Table 1 and Figure 1.
Results
Following hemadsorption sessions, significant clinical and biochemical improvement was observed: serum bilirubin levels decreased from 24.1 mg/dl to 5.6 mg/dl and remained stable, with further spontaneous reduction in subsequent days. ALT/SGPT decreased from 335 U/L to 59 U/L. AST/SGOT decreased from 183 U/L to 92 U/L. PCT levels declined from 23.2 μg/l to 9.54 μg/l.
The patient’s respiratory distress resolved, and she became fully conscious and orientated. Haemodynamic stability was achieved, and she was transferred to the general ward on January 13.
| Day | Bilirubin (mg/dl) | ALT/SGPT (U/L) | AST/SGOT (U/L) | PCT (µg/L) |
| 1 | 24.1 | 335 | 183 | 23.20 |
| 2 | 15.0 | 200 | 140 | 18.00 |
| 3 | 9.0 | 150 | 120 | 12.00 |
| 4 | 7.2 | 100 | 100 | 10.50 |
| 5 | 5.6 | 59 | 92 | 9.54 |
Table 1: Laboratory parameters from Day 01- Day 05 following Hemadsorption sessions.
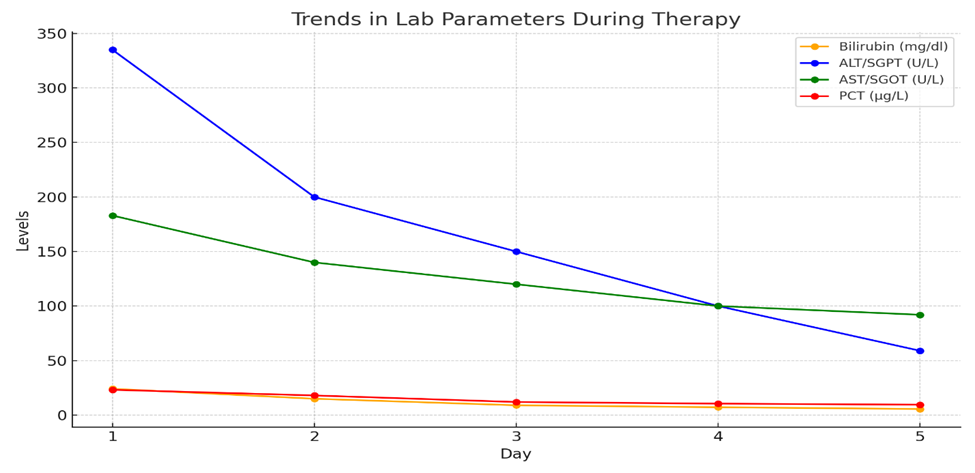
Figure 1: Laboratory parameters from Day 01- Day 05 following Hemoadsorption sessions.
The chart above illustrates the rapid improvement in bilirubin, ALT/SGPT, AST/SGOT, and PCT levels over the 5-day course of hemoadsorption therapy. Notable decreases in bilirubin and inflammatory markers highlight the efficacy of the treatment.
Patient Follow-Up
The patient experienced a complication-free hospital course and was discharged home on January 26, 2024. Although long-term follow-up data were not available, the prognosis appeared favourable given the significant improvements observed during hospitalization. Discussions on relapse risks and the need for continued vigilance were communicated to the patient and her family.
Discussion
Cytokine adsorption therapy played a pivotal role in this patient’s recovery by rapidly reducing inflammatory markers and bilirubin levels, thereby mitigating the cytokine storm associated with sepsis (Schädler et al., 2017). The absence of anticoagulation during RRT minimized bleeding risks without causing complications. The synergistic effects of antibiotics and supportive care also contributed to the positive outcome, highlighting the importance of a multimodal treatment approach. Comparative studies have demonstrated the efficacy of hemoadsorption in sepsis management, particularly in reducing cytokine load, improving haemodynamics, and supporting organ recovery. However, limitations such as cost implications and the need for long-term efficacy data warrant further investigation. Future studies should explore the comparative effectiveness of hemoadsorption versus other therapies, such as high-volume hemofiltration and extracorporeal membrane oxygenation (ECMO).
Conclusions
In this patient with sepsis, AKI, and acute fulminant hepatitis, hemoadsorption therapy combined with standard care led to rapid clinical improvement and stabilization of inflammatory markers. This case underscores the safety, ease of use, and efficacy of hemoadsorption as a valuable adjunct in managing complex sepsis cases.
Authors of this article
- Dr. Mohammad Golam Azam, MD, Associate Professor, Department of Gastrointestinal, Hepatobiliary and Pancreatic Disorders (GHPD)
- Prof. Dr. A.S.M. Areef Ahsan, FCPS, MD, Professor, Head, Department of critical care medicine
- Dr. Mehruba Alam Ananna, FCPS, Associate professor, Department of nephrology and dialysis
- Dr. Israt Jahan, FCPS, Registrar, Department of critical care medicine.
References
- Friesecke, S., Träger, K., Schittek, G. A., Molnar, Z., Bach, F., Kogelmann, K., Bogdanski, R., Weyland, A., Nierhaus, A., Nestler, F., Olboeter, D., Tomescu, D., Jacob, D., Haake, H., Grigoryev, E., Nitsch, M., Baumann, A., Quintel, M., Schott, M., … Brunkhorst, F. M. (2019). International registry on the use of the CytoSorb® adsorber in ICU patients: Study protocol and preliminary results. Medizinische Klinik – Intensivmedizin Und Notfallmedizin, 114(8), 699–707. https://doi.org/10.1007/s00063-017-0342-5
- Kogelmann, K., Jarczak, D., Scheller, M., & Drüner, M. (2017). Hemoadsorption by CytoSorb in septic patients: A case series. Critical Care, 21(1). https://doi.org/10.1186/s13054-017-1662-9
- Schädler, D., Pausch, C., Heise, D., Meier-Hellmann, A., Brederlau, J., Weiler, N., Marx, G., Putensen, C., Spies, C., Jörres, A., Quintel, M., Engel, C., Kellum, J. A., & Kuhlmann, M. K. (2017). The effect of a novel extracorporeal cytokine hemoadsorption device on IL-6 elimination in septic patients: A randomized controlled trial. PLoS ONE, 12(10). https://doi.org/10.1371/journal.pone.0187015
- Singer, M., Deutschman, C. S., Seymour, C., Shankar-Hari, M., Annane, D., Bauer, M., Bellomo, R., Bernard, G. R., Chiche, J. D., Coopersmith, C. M., Hotchkiss, R. S., Levy, M. M., Marshall, J. C., Martin, G. S., Opal, S. M., Rubenfeld, G. D., Poll, T. Der, Vincent, J. L., & Angus, D. C. (2016). The third international consensus definitions for sepsis and septic shock (sepsis-3). In JAMA – Journal of the American Medical Association (Vol. 315, Issue 8, pp. 801–810). American Medical Association. https://doi.org/10.1001/jama.2016.0287
- White, J. A. (2007). Pre-pump arterial pressure = what is going on with the patient’s access. Post-pump arterial pressure = what is going on inside the dialyzer. Why is PBE an important tool? PBE Pressure of Blood Entry Another way of illustrating post-pump arterial pressure.

