Abstract
Metaplastic squamous cell breast carcinoma represents a very rare subtype of breast cancer. Histologically metaplastic carcinoma is characterized by the presence of at least two cellular types, typically epithelial and mesenchymal components.1. Metaplastic breast carcinoma (MpBC) is especially uncommon in young individuals and overall, the prognosis and outcome are poor. The usual treatment protocol for metaplastic squamous carcinoma of the breast needs a multidisciplinary approach including chemotherapy and surgery. This case report highlights the clinical presentation of a 35 year-old married woman who noticed a lump in her right breast and came for evaluation within a month of this symptom. Histopathological examinations revealed metaplastic breast carcinoma with squamous differentiation. In this case report, we have mainly discussed the clinical presentation of metaplastic breast carcinoma with squamous differentiation and the importance of a multidisciplinary treatment approach.
Keywords: Invasive breast carcinoma, Metaplastic, Triple negative tumor, Radical mastectomy.
Introduction:
Metaplastic carcinoma of the breast (MCB) was first described in 19731 and was defined as a mammary carcinoma with mixed epithelial and sarcomatoid components. Instead of using the lymphatic system to spread, there is a high risk of metastatic dissemination to the lung and bone tissue.2
Metaplastic squamous cell breast cancer is an extremely rare subtype, accounting for less than 1% of all invasive breast cancers. This rare and aggressive metaplastic breast cancer (MpBC), which makes up between 0.2% and 5.0% of all breast cancers, has the worst prognosis of all breast cancers and is a major contributor to breast cancer mortality globally.3
The World Health Organization (WHO) further categorizes metaplastic breast cancer into the following subgroups: mixed metaplastic carcinoma, myoepithelial carcinoma, low-grade adenosquamous carcinoma, fibromatosis-like metaplastic carcinoma, squamous cell carcinoma, and spindle cell carcinoma.4
The majority of breast cancer cases have an unknown source. However, a number of risk factors for the condition have been identified, including female gender, advancing patient age, a history of breast cancer in the patient’s family at a young age, early menarche, late menopause, older age at first live birth, prolonged hormone replacement therapy, prior exposure to therapeutic chest wall irradiation, benign proliferative breast disease, and genetic mutations, such as those in the BRCA1/2 genes.5
They frequently appear as palpable breast masses with poorly defined borders on mammography and have dimensions ranging from 1.2cm to >10 cm. They are typically substantial in size.6Metaplastic breast carcinoma is usually negative for ER, PR, and HER-2 (Triple negative). Triple-negative breast cancer (TNBC) doesn’t have estrogen or progesterone receptors and also make too little or none of the HER2 protein. Because the cancer cells don’t have these proteins, hormone therapy and drugs that target HER2 are not helpful, so chemotherapy (chemo) is the main systemic treatment option. And even though TNBC tends to respond well to chemo initially, it also tends to come back (recur) more frequently than other breast cancers.
Treatment options for metaplastic breast carcinoma are surgery (either radical mastectomy or breast conservative surgery), chemotherapy and hormonal therapy, and radiation therapy.7
But after even successful treatment overall prognosis and survival rates are very poor.
Case presentation:
A 35-year-old married Bangladeshi lady noticed a painless lump in her right breast’s upper and inner quadrant 1 month ago. After the initial presentation, she underwent a breast examination and routine ultrasonography of both breasts. Ultrasound of the breast revealed a fairly large irregular complex mass measuring about (80 × 51mm, 04 mm from the skin).
Then mammography of both breasts revealed BIRADS category 6 lesions in the upper & inner quadrants of the right breast.
Table 1: Breast imaging reporting and data system (BIRADS)
| Category | Interpretation |
| Category 0 | Incomplete. Needs additional imaging evaluation. |
| Category 1 | Negative. No detectable pathology is seen. |
| Category 2 | Benign lesion (lesion, vascular calcification, architectural distortion from previous operation) |
| Category 3 | Probable benign lesion, less than 2% chance of malignancy. Short interval follow-up. |
| Category 4 | Suspicious lesion for malignancy. 2-90% chance of malignancy. Biopsy is recommended. |
| Category 5 | Highly suggestive of malignancy. More than 95% chance of malignancy. Biopsy is recommended. |
| Category 6 | Known biopsy-proven malignant breast lesion. |
Then she underwent a Tru-cut biopsy which revealed a malignant neoplasm composed of poorly differential ductal with squamous differentiation.
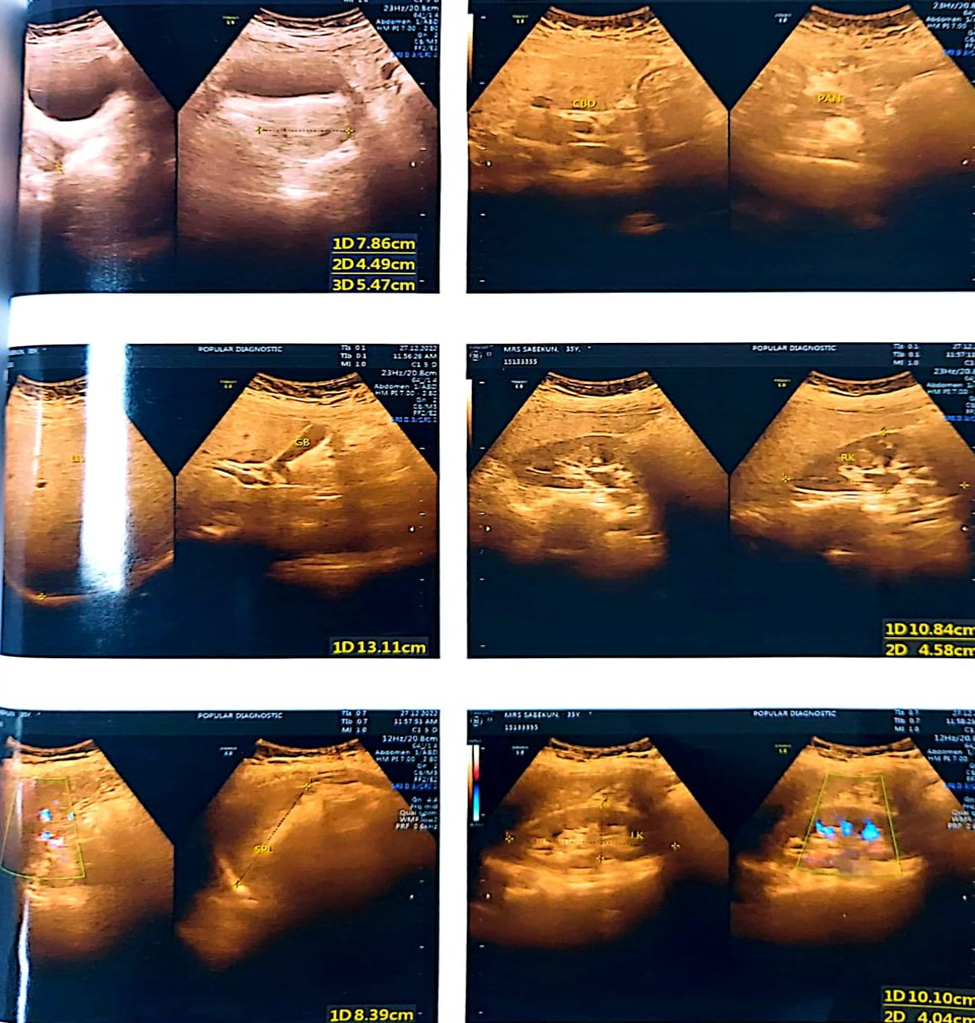
Figure 1: Imaging of Metaplastic carcinoma
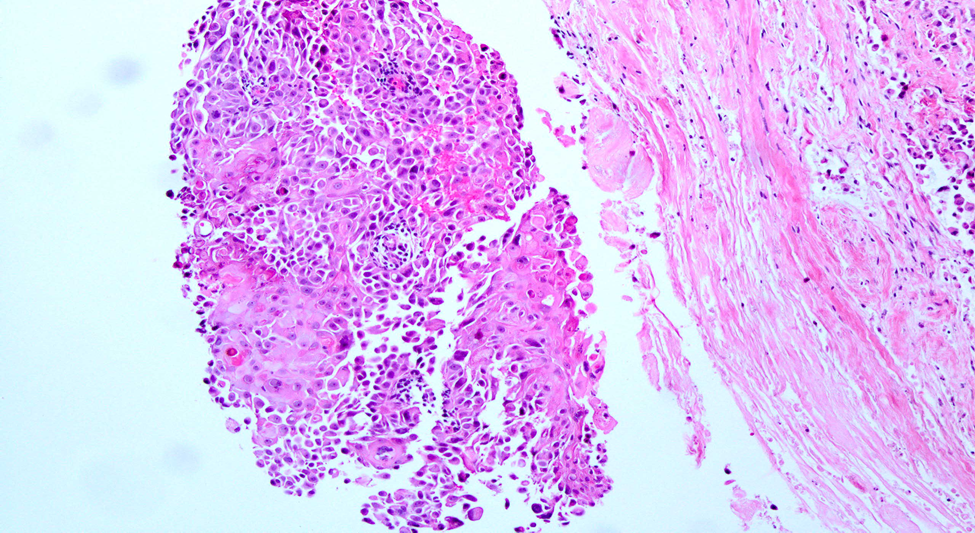
Figure 2: Metaplastic carcinoma with squamous differentiation. Courtesy Huina Zhang, M.D, Ph. D.
The usual treatment protocol for this type of metaplastic carcinoma is multidisciplinary. Procedure including chemotherapy and surgery was planned for this patient.
Before starting chemotherapy immunohistochemistry for ER, PR, and HER-2 was done and it was negative.
Triple-negative tumors are difficult to treat using medications that target these characteristics of cancer cells. Chemotherapy is frequently used in the first stages of treatment to reduce tumor size. Following this course of treatment, surgery, and radiation therapy are used.8
Initially, chemotherapy was given. Then total mastectomy of the right breast was done. After the mastectomy of the right breast total breast including the nipple, skin, and axillary tail of the breast was sent for histopathology. Histopathological findings were metaplastic carcinoma with squamous differentiation, the tumor is classified as grade 2 with pT2N0MX and RCB class 2.
Discussion:
Metaplastic breast carcinoma is an uncommon form of breast cancer primarily found in older women. Unfortunately, the prognosis for this type of cancer is typically poor.
Due to the absence of the progestin receptor, estrogen receptor, and human epidermal growth factor receptor 2 activities, metaplastic breast cancer is characterized as triple negative, which can make treatment more difficult.9 Histologically, this type of cancer is characterized as a poorly differentiated tumor that can contain a mix of different cell types.10
While it is rare for metaplastic carcinoma to occur in younger individuals, our patient, a 35-year-old woman, recently discovered a painless lump in her right breast that appeared one month ago. She took ayurvedic therapy from a local practitioner as treatment for the lump; hence, the standard treatment was delayed further.
She underwent an ultra-sonogram of both breasts, the lump appeared as an irregular complex mass, after that mammography of both breasts along with tumor marker was done. Mammography showed BIRADS category 6 lesions. Then Tru-cut biopsy was done which revealed a malignant neoplasm composed of poorly differential ductal with squamous differentiation. Metaplastic breast cancers are triple negative and unresponsive to some useful chemotherapeutic agents. Breast conservative surgery and radical mastectomy are two surgical options for breast carcinoma. In metaplastic breast carcinoma, radical mastectomy is the treatment of choice. For this patient, radical mastectomy was performed, followed by a biopsy. The histopathology revealed that the patient had metaplastic breast carcinoma with squamous differentiation. The tumor is classified as grade 2 with pT2N0MX and RCB class 2.
In the early-stage if the TNBC tumor is small enough to be removed by surgery, then breast-conserving surgery or a mastectomy with a check of the lymph nodes may be done. In certain cases, such as patients presenting a large tumor or if the lymph nodes are found to have cancer, radiation may follow surgery. Additional chemo post-surgery may also be prescribed as adjuvant chemotherapy to reduce the chances of recurrence of the cancer.
Women who are BRCA mutation positive and at surgery are found to have a tumor larger than 2cm but no bigger than 5cm OR 1 to 3 axillary (underarm) lymph nodes with cancer, the targeted drug delivery might be given for a year after adjuvant chemo. This protocol can help some women live longer.
Chemotherapy is often given before surgery (neoadjuvant chemotherapy) by itself or with drug to shrink a large tumor and/or lymph nodes with cancer. If cancer is still found in the tissue removed by surgery after neoadjuvant chemo has been given to women who have a BRCA mutation to help lower the chance of the cancer recurring.
In stage IV triple-negative breast cancer, chemotherapy is often used first when the cancer has spread to other parts of the body (stage IV). Common chemo drugs used include anthracyclines, taxanes, capecitabine, gemcitabine, eribulin, and others. Chemo drugs might be used alone or in combination.
For women with TNBC who have a BRCA mutation and whose cancer no longer responds to common breast cancer chemo drugs, for advanced TNBC in which the cancer cells have the PD-L1 protein, the first line of treatment may be immunotherapy plus chemo. The PD-L1 protein is found in about 1 out of 5 TNBCs.
Also, for TNBC in which the cancer cells show high levels of gene changes called microsatellite instability (MSI) or changes in any of the mismatch repair (MMR) genes (MLH1, MSH2, MSH6, and PMS2), immunotherapy with the drug might be used. Pembrolizumab might also be an option for TNBC that has a high tumor mutational burden (TMB-H) which is a measure of the number of gene mutations (changes) inside the cancer cells. Cells that have many gene mutations (a high TMB) might be more likely to be recognized as abnormal and attacked by the body’s immune system.
Surgery and radiation may also be options in certain situations.
Currently, there are no specific guidelines for the management of TNBC. Systemic chemotherapy continues to be the mainstay of treatment, as the majority of TNBCs tend to be exquisitely sensitive to chemotherapy. However, how this systemic therapy specifically impacts loco regional control remains less clear. Radiation therapy is indicated for the majority of patients who undergo BCT and is also indicated for a sub-set of patients following mastectomy if high-risk features for loco regional recurrence exist, for example multiple positive lymph nodes, tumors >5 cm, presence of lymphovascular invasion or positive surgical margins. There are no tumor subtype-specific guidelines regarding adjuvant radiation therapy. Given that adjuvant radiation therapy is used for local control and TNBCs appear to have a higher incidence of loco regional recurrence, there has been recent interest in determining whether TNBC, a specific subtype of breast cancer, is likely to benefit from radiation therapy regardless of surgical intervention. Therefore, several retrospective studies have analyzed the role of radiation therapy in TNBC, but their findings are conflicting.
Prognosis and outcome:
The overall outcome of metaplastic carcinoma of the breast is very poor. The five-year survival rate of metaplastic breast carcinoma is about 55%.8
Conclusion
Histopathological examinations revealed metaplastic breast carcinoma with squamous differentiation. In this case report, we have discussed a clinical presentation of metaplastic breast carcinoma with squamous differentiation.
Author of this article
Dr. Fahmida Alam, MBBS, BCS (Health), FCPS (Radiotherapy), Consultant, Department of Oncology, Chittagong Medical College & Hospital, Chittagong
Reference:
- Huvos AG. Metaplastic breast carcinoma. NY J Med. 1973;73:1078-82.
- McKinnon E, Xiao P. Metaplastic carcinoma of the breast. Archives of Pathology and Laboratory Medicine. 2015 Jun 1;139(6):819-22.
- Reddy TP, Rosato RR, Li X, Moulder S, Piwnica-Worms H, Chang JC. A comprehensive overview of metaplastic breast cancer: clinical features and molecular aberrations. Breast Cancer Research. 2020 Dec;22(1):1-1.
- El Zein D, Hughes M, Kumar S, Peng X, Oyasiji T, Jabbour H, Khoury T. Metaplastic carcinoma of the breast is more aggressive than triple-negative breast cancer: a study from a single institution and review of literature. Clinical breast cancer. 2017 Aug 1;17(5):382-91.
- Carlson RW, Allred DC, Anderson BO, Burstein HJ, Carter WB, Edge SB, Erban JK, Farrar WB, Forero A, Giordano SH, Goldstein LJ. Invasive breast cancer. Journal of the National Comprehensive Cancer Network. 2011 Feb 1;9(2):136-222.
- McCart Reed AE, Kalaw EM, Lakhani SR. An update on the molecular pathology of metaplastic breast cancer. Breast Cancer: Targets and Therapy. 2021 Feb 26:161-70.
- Shah DR, Tseng WH, Martinez SR. Treatment options for metaplastic breast cancer. International Scholarly Research Notices. 2012;2012.
- Metaplastic breast cancer. (n.d.). MD Anderson Cancer Center. Retrieved September 15, 2023, from https://www.mdanderson.org/cancer-types/breast-cancer/metaplastic-breast-cancer.html
- Arekemase H, Mohammed O, Zafar U, Manpreet K, Maghari A, Osmani MA, Zafar U. Metaplastic Breast Carcinoma Presenting as a Mixed Solid and Cystic Lesion. Cureus. 2022 Feb 8;14(2).
- Al Sayed AD, El Weshi AN, Tulbah AM, Rahal MM, Ezzat AA. Metaplastic carcinoma of the breast clinical presentation, treatment results, and prognostic factors. Acta Oncologica. 2006 Jan 1;45(2):188-95

